How AI Is Quietly Improving Health and Medicine
Progress in health and medicine rarely arrives as a single breakthrough. More often, it unfolds through incremental improvements — earlier detection, clearer data, better tools, and systems that support clinicians and researchers in making more informed decisions.
In recent years, artificial intelligence has begun to play a quiet but increasingly meaningful role in this process. Not as a replacement for doctors or scientists, but as an enabling layer — one that helps process complexity, recognize patterns, and extend human capacity.
What follows are specific, real developments where AI is already contributing to health and medical progress today — often without widespread public attention.
Mapping human biology at unprecedented scale
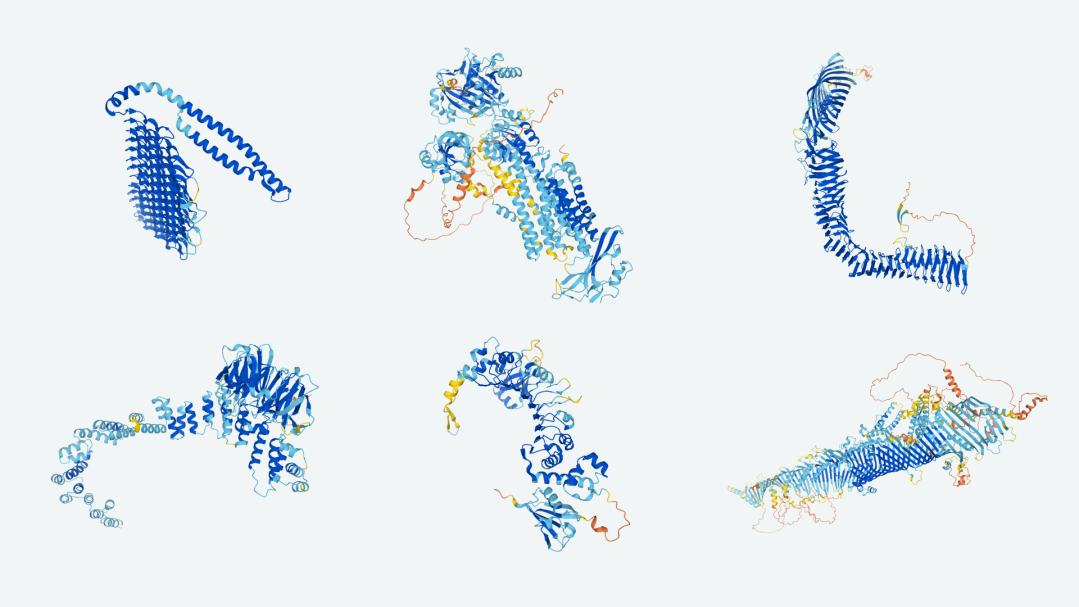
One of the most consequential advances in modern biology has been the use of AI to predict the structure of proteins — the fundamental building blocks of life.
Through the AlphaFold project developed at DeepMind, AI systems have been used to predict the structures of hundreds of millions of proteins — a task that previously required years of laboratory work per protein.
The scientific leadership behind this effort includes Demis Hassabis, whose background spans neuroscience, artificial intelligence, and cognitive science, alongside large interdisciplinary teams of biologists, physicists, and engineers.
Understanding protein structures is foundational for drug discovery, rare disease research, and fundamental biology. By making this data openly available, AlphaFold has significantly accelerated research across the life sciences. This is not a projected benefit — it is already reshaping how biological research is conducted.
Earlier and more accurate disease detection
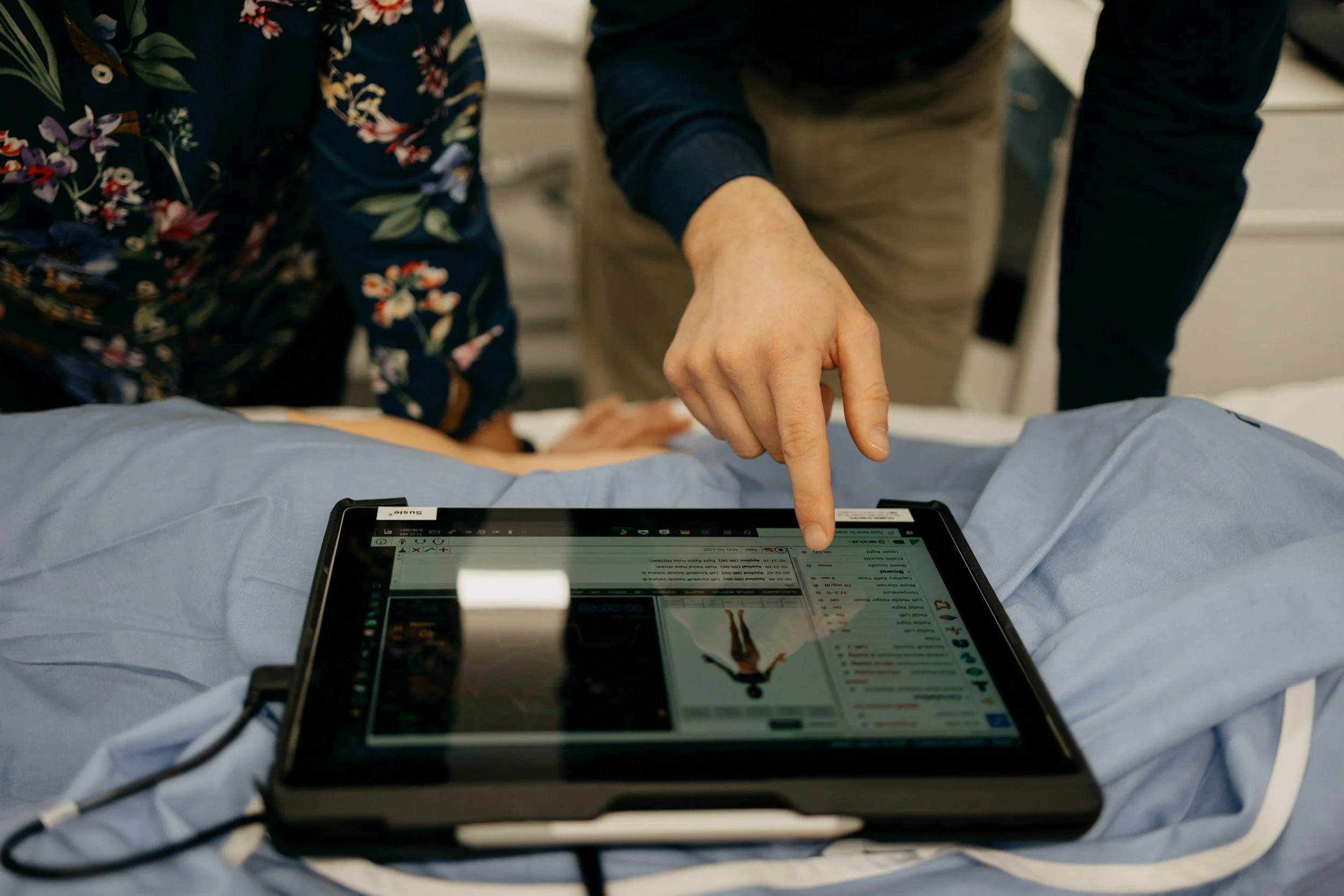
AI-assisted imaging systems are increasingly supporting clinicians in detecting diseases at earlier stages, particularly in areas such as breast cancer screening, lung cancer detection, retinal disease identification, and cardiovascular risk assessment.
Rather than operating independently, these systems function as decision-support tools — analyzing large volumes of images and highlighting areas that warrant closer human review.
Much of this progress has emerged through large-scale clinical research and deployment within national healthcare systems, including screening programs in parts of Europe and North America.
Earlier detection often allows for less invasive treatment and improved outcomes. Even modest gains in detection accuracy can have meaningful effects at population scale.
AI-assisted drug discovery reaching clinical trials
AI is now playing a measurable role in parts of the drug discovery process.
In recent years, several drug candidates identified or optimized using AI-assisted methods have progressed into clinical trials through collaborations between biotech firms, academic research institutions, and pharmaceutical partners — particularly in the United States and Europe.
AI systems help researchers identify promising molecular structures, explore drug–target interactions, and reduce unproductive trial pathways.
Drug development is slow, costly, and uncertain. Even incremental improvements in efficiency can shorten development timelines and help treatments reach patients sooner.
Revealing patterns humans struggle to detect consistently
In fields such as cardiology, oncology, and neurology, AI systems are being used to analyze complex datasets — including medical imaging, physiological signals, and patient histories — to identify subtle patterns that can be difficult for humans to detect consistently.
These systems do not make clinical decisions. Instead, they surface signals that clinicians can interpret, validate, and act upon.
This work is taking place across research hospitals and medical centers worldwide as part of broader efforts to improve diagnostic accuracy and risk assessment.
By expanding what is visible within complex data, AI supports earlier intervention and more informed clinical judgment without removing human oversight.
Medical imaging beyond diagnosis
Beyond initial detection, AI is increasingly used to support how diseases are monitored and treated over time. In areas such as oncology, neurology, and cardiology, AI-assisted imaging systems help clinicians compare scans taken weeks or months apart — highlighting subtle changes that may indicate whether a treatment is working or needs adjustment.
For example, in cancer care, AI tools can assist in tracking tumor response across successive imaging studies, while in surgical planning they can help map anatomical structures more precisely before an intervention. Rather than replacing clinical judgment, these systems provide an additional layer of consistency and clarity in complex cases.
When conditions evolve slowly or treatments require fine calibration, small insights can have significant consequences. By supporting more adaptive and precise care, AI contributes to better-informed decisions throughout a patient’s treatment journey.
Expanding access in under-resourced settings
In healthcare settings where medical specialists are limited, AI-assisted screening tools are increasingly being used to support access to basic diagnostics. These systems — for example, those used to analyze retinal images for diabetic eye disease or chest X-rays for tuberculosis — help identify patients who may need further evaluation by a clinician.
Such tools are now used globally, including in high-income healthcare systems, but their impact is particularly significant in regions where specialist access is uneven. Through collaborations between research institutions, healthcare providers, and public health organizations, AI is helping redistribute medical expertise rather than replace it. Even incremental improvements in early detection and access can have meaningful long-term effects on public health.
Supporting medical research itself
AI is also being used to help researchers navigate the scale and complexity of modern medical knowledge. Applications include analyzing large biomedical datasets, identifying connections across studies, and assisting with literature synthesis and research planning.
Why it matters: Progress depends not only on discovery, but on integration — ensuring knowledge compounds rather than fragments.
What this progress represents
We are living in a remarkable period of human history. Never before have science, medicine, and technology offered such a deep understanding of how the human body works — and how it can be protected, supported, and sustained over time. From earlier disease detection to more precise treatments and a growing body of knowledge around prevention, longevity, and health, the trajectory is unmistakably positive.
While no single technology offers guarantees, the combination of scientific research, medical expertise, and intelligent tools is steadily improving both the length and quality of human life. For the first time, extending healthy lifespan is not a philosophical idea, but an active area of global effort. In this sense, we are fortunate to live at a moment when progress is not hypothetical, but measurable — built quietly, carefully, and with genuine promise for the future.